Details
-
Change Request
-
Resolution: Unresolved
-
Medium
-
National Directory of Healthcare Providers and Services (NDH) (FHIR)
-
1.0.0-ballot
-
Patient Administration
-
NDH Base Organization Profile
NDH Base OrganizationAffiliation Profile
NDH Base Practitioner Profile
NDH Base PractitionerRole
Description
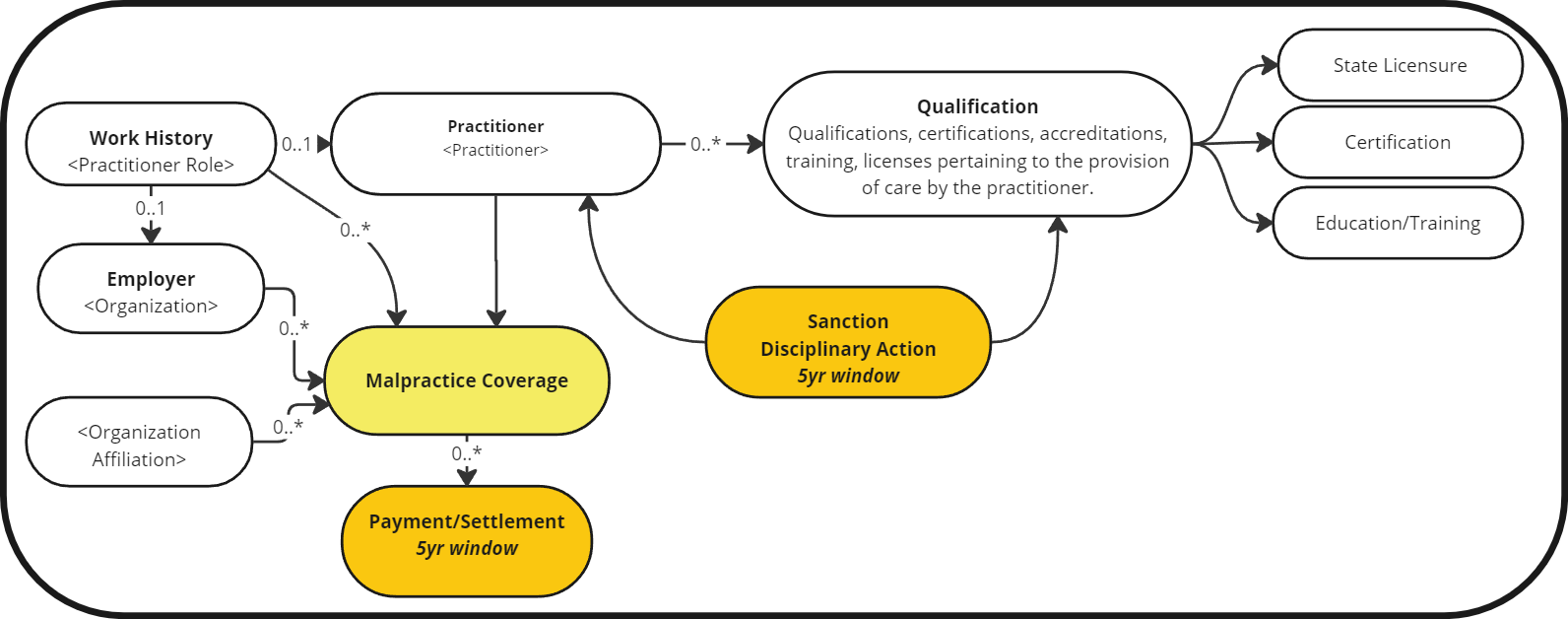
In the credentialing domain, there are three elements not captured in the NHD IG or US Core resources.
Practitioner credentialing domain consists of the following entities:
- Practitioner
- State Licenses
- Certifications
- DCS
- DEA
- Education & Training
- Sanctions (Disciplinary Actions)
- State
- Medicaid
- Medicare
- Malpractice
- Settlement/Payment (5yr window)
- Work History (5yr window)
Initial mapping to NHD resources indicates the following:
- Practitioner: Practitioner
- State Licenses: Practitioner.Qualification
- Certifications: Practitioner.Qualification
- DCS
- DEA
- Education & Training: Practitioner.Qualification
- Work History (5yr window): PractitionerRole(WorkHistory) + Organization(Employer)
- Sanctions/Disciplinary Actions
- State
- Medicaid
- Medicare
- Malpractice Coverage
- Settlements/Payments (5yr window)
Gaps identified for this use case are the following:
- Sanctions/Disciplinary Actions
- State
- Medicaid
- Medicare
- Malpractice Coverage
- Settlement/Payment (5yr window)
When looking at Malpractice Insurance/Coverage initial mindset is to look at Coverage or Insurance Plan.
- Coverage is of the context of the patient and requires one beneficiary which referneces a Patient.
- An Insurance Plan may be a good fit.
When looking at Malpractice Payment/Settlement initially one may look at CliamResponse, PaymentNotice, or Payment Reconciliation.
- The PaymentNotice resource is used to indicate that a payment has or is about to occur. The resource is used commonly when tracking of payment occurrences is required for regulatory or business purposes.
- The ClaimResponse resource is an insurer's adjudication and/or authorization of a set of healthcare-related goods and services for a patient against the patient's insurance coverages and does not indicate that payment has occured.
Solutions to gaps: (Resource attributes to be defined)
- Sanctions/Disciplinary Actions applicable for a given period which is within the Practitioner.Qualification period:
- Practitioner
- Practitioner.Qualification
- Malpractice Coverage may contain zero to many Payments/Settlements (history needed is past five years)
- Practitioner Role may have 0..* Malpractice Coverage
- Practitioner Role's organization may have 0..* Malpractice Coverage
- Organization Affiliation may have 0..* Malpractice Coverage
Definitions
- Malpractice Settlements/Payments:
- The organization obtains confirmation of the past 5 years of malpractice settlements from the malpractice carrier or queries the National Practitioner Databank (NPDB). The 5-year period may include residency or fellowship years. The organization is not required to obtain confirmation from the carrier for practitioners who had a hospital insurance policy during a residency or fellowship
- Sanctions (State, Medicare, Medicaid)
https://www.npdb.hrsa.gov/software/sampleResponseFiles.jsp
https://www.providertrust.com/blog/what-is-the-difference-between-a-sanction-and-exclusion/
- The organization verifies state sanctions, restrictions on licensure and limitations on scope of practice in all states where the practitioner provides or has provided care to members for the most recent 5-year period available. If practitioners were licensed in more than one state in the most recent 5-year period, the query must include all states in which they provided care.
- A sanction (also referred to as a medical sanction) is the result of a disciplinary action taken against an individual’s license by a state administrative board- commonly by a state licensing board. Sanctions can be imposed for many reasons but are primarily the result of patient abuse, criminal convictions related to diversion of controlled substances, or healthcare fraud.
- An exclusion, however, is the result of an extreme sanction which is issued by the HHS OIG (Office of Inspector General). Exclusions are typically reserved for those who pose a high risk to patients or a program’s integrity.
